Coronavirus (COVID-19) Updates by Dr. Bruce Feinberg
Choose your favorite entertainment genre: sci-fi, fantasy, noir, suspense, pretty much anything other than rom-com and imagine you have arrived at the final chapter, episode, or scene- that is where we are now in the story of the SARS-CoV2 pandemic. Like that terrifying roller coaster ride that you allowed yourself to be persuaded to go on where the longest, steepest, fastest drop is the one that remains, you are in the first car staring down from the apex. Regardless of the proverb that resonates: “it’s darkest before the dawn,” “what doesn’t kill you makes you stronger,” we are at that moment, the denouement of this story, when we emerge from anguish, hopelessness, and despair into transcendent joy. Such moments of incredible tension may produce a pleasant endorphin rush when they are brief and under our control in a movie, TV series, or book, but when real and out of our control they can be unbearable. In today’s update, I hope to give you back control of this roller coaster ride called COVID.
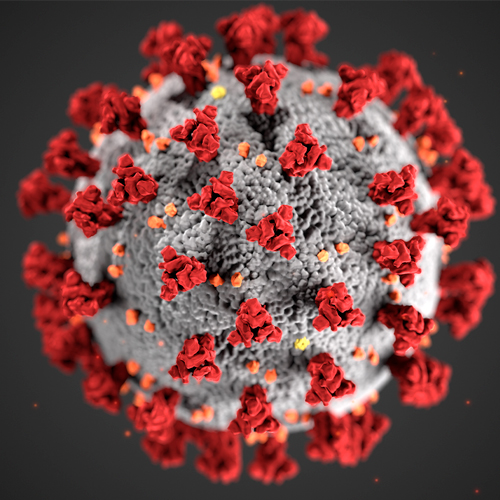
One of the more consistent comments from those reading these updates is not only how they benefit your personal understanding of the issues presented but more importantly how they provide a template for you to share that understanding with family and friends. The complexity of some of the pandemic-related issues begs for metaphors, analogies, graphics, and images to aid understanding. In this update, I share two such visual/conceptual aids to better understand the two most prevalent COVID topics, the promise of the mRNA vaccines and how we protect ourselves for the next six months while most of us wait until we are at the front of the vaccination line.
We are nine months into the pandemic and another six months feels overwhelming. Your brain tells you that you can’t quit but you think you’ve hit the wall, emotionally, spiritually, physically depleted. Like the marathon runner at the 22nd-mile mark, the wall stands before you, and with each passing step, it grows taller and more formidable. To conquer these final miles, endurance athletes are told to consider the notion that it’s not about “breaking through the wall,” but instead never getting to the wall in the first place. Although the vaccine might be six months away for most of us, we have control over COVID now. The swiss cheese defense metaphor, described below, provides the conceptual framework and reassurance that we can persevere. The wall is only an illusion, the finish line is real. The mRNA vaccine is the finish line and understanding how it is different from a traditional vaccine and how it has been proven both safe and effective in less than a year of study, described below, will help you keep your focus on the finish. It’s important to understand that the mRNA vaccine simply mimics the viral infection process. SARS CoV2 is an RNA virus. After the spike protein binds to the ACE receptor on cells lining the respiratory tract the viral RNA penetrates the cell and, like the cell’s own RNA, tricks the cell into manufacturing viral protein like the spike protein. The immune cells of the host subsequently recognize the viral spike protein and create antibodies against it. We do not become genetically modified organisms when we get vaccinated mRNA.
The multilayered “Swiss cheese” model was devised in the 1990s to improve industrial safety. Ian Mackay, a virologist at the University of Queensland, recently adapted it for the coronavirus pandemic. “It’s important to use more slices to prevent those volatile holes from aligning and letting virus through,” he said.
Updated November 5, 2020
Although our thoughts and feelings in the coming days and possibly weeks may be dominated by angst over election results, our lives in the coming months and possibly years will be dominated by COVID. The stark reality of this virus is that both effective vaccines and effective treatments will need to be readily accessible worldwide for the resumption of normalcy as we once knew it. A future state in which the impact of the SARS CoV2 virus is no different from influenza is likely years away. The world will need several different vaccines to fight the COVID-19 pandemic: given the sheer size of global need, variations in effects on different populations, and possible limits of effectiveness in their first iterations.
The first iteration vaccines have used unconventional methods to expedite development based on new and largely unproven technology platforms designed to produce vaccines at speed. They include messenger RNA (mRNA) technology used by Moderna and Pfizer and inactivated cold virus platforms used by Oxford University/AstraZeneca, Johnson & Johnson, and CanSino Biologics (whose vaccine has been approved for military use in China). Merck in September started testing a COVID-19 vaccine based on a weakened measles virus that delivers genes from the new coronavirus into the body to stimulate an immune response to the coronavirus. Of these, only the technology offered by J&J and CanSino, that use cold viruses as vectors to deliver coronavirus genetic material, has ever produced a licensed vaccine – and that is for Ebola. The second iteration vaccines, with late-stage trial results expected in the first half of 2021, are heavily skewed toward approaches that use established techniques and have produced successful vaccines in the past.
These 2nd iteration vaccines rely on established methodologies: 1. using a killed or inactivated version of the disease-causing virus to provoke an immune response, such as those used to make flu, polio, and rabies vaccines; or 2. protein-based vaccines that use purified pieces of the virus to spur an immune response like vaccines for whooping cough, pertussis, and shingles. Sanofi is developing a protein-based COVID-19 vaccine employing the same approach it uses for its Flublok seasonal flu vaccine. Sanofi expects to start the final phase of testing in early December, with approval targeted in the first half of 2021. Novavax has not yet produced a licensed vaccine, it is using similar purified protein technology and expects to start a late-stage U.S. trial involving 30,000 volunteers in late November. Inactivated virus vaccines being developed by Chinese researchers are among the few 1st iteration vaccines using a traditional technique. Other second-wave developers are making vaccines based on virus-like particles (VLPs), which mimic the structure of the coronavirus but contain no genetic material from it. VLP vaccines can be produced in a variety of different types of cells, including mammal, bacterial, insect, yeast, and plant cells. This approach has been used to develop vaccines for hepatitis B and human papillomavirus. Quebec’s Medicago is testing a VLP vaccine grown in tobacco plants with the backing of tobacco company Philip Morris, it plans to begin mid-stage trials of its vaccine next month and aims to make up to 1 billion doses a year by 2023. Other researchers are looking at alternative delivery methods, such as the nasal spray vaccine being developed by a team at Hong Kong University which is based on a modified flu virus.
Regardless of the conventional or novel methodology used for vaccine development, the vaccine approval process is a complex enterprise that requires large clinical trials with tens of thousands of volunteers randomized to vaccine or placebo cohorts. Although it is easier and faster to prove efficacy when community spread of the virus is rampant, as has been the case in the US and EU, those volunteering may not be engaging in the risky behaviors that result in viral transmission. Only when there are statistically meaningful differences in viral infection rates between the vaccine and sham cohorts can the vaccines be evaluated for approval, but such approvals may not be informed by long-term proof of safety. Even when there is proof of both safety and efficacy will enough of the population willingly vaccinate to generate the herd immunity needed to eradicate the virus? Such concerns make the need for effective treatments as critical as the need for effective vaccines.
Although remdesivir and corticosteroids have reduced COVID mortality their benefit is modest. Antiviral prevention strategies administered at the earliest recognition of infection, akin to Tamiflu, will be critical to the comprehensive strategy. REGN-COV2, the drug administered to president Trump, is a combination of monoclonal antibodies designed specifically to block infectivity. In the ongoing phase 2/3 seamless trial in the COVID-19 outpatient setting, REGN-COV2 met the primary and key secondary endpoints with the latest data from the trial including an analysis of 523 patients, in addition to the first 275 patients previously reported.
The virologic results showed:
- The average daily change in viral load through day 7 in patients with high viral load was a 0.68 log10 copies/mL greater reduction with REGN-COV2 compared with placebo (combined dose groups; p<0.0001). There was a 1.08 log greater reduction with REGN-COV2 treatment by day 5, which corresponds to REGN-COV2 patients having, on average, a greater than 10-fold reduction in viral load, compared with placebo.
- In the overall patient group with detectable virus at baseline, the average daily reduction in viral load through day 7 was a 0.36 log10 copies/mL greater reduction with REGN-COV2, compared with placebo (combined dose groups; p=0.0003).
- Patients with a higher viral load at baseline and/or no detectable antibodies at baseline (suggesting their bodies had not yet mounted an effective immune response), derived greater benefit from REGN-COV2 therapy.
While the clinical results in the overall population showed:
- Treatment with REGN-COV2 reduced COVID-19 related medical visits by 57% through day 29 (2.8% combined dose groups; 6.5% placebo; p=0.024).
- Treatment with REGN-COV2 reduced COVID-19 related medical visits by 72% in patients with 1 or more risk factor (combined dose groups; nominal p=0.0065).
Investigators noted that the results showed no significant difference in virologic or clinical efficacy between the REGN-COV2 high dose (8 grams) and low dose (2.4 grams). Regeneron said that it is reviewing potential changes to dosing in the ongoing outpatient trial given the current limited supply of the drug. REGN-COV2 was generally well tolerated in the trial but it did have more frequent severe adverse events (AEs) in patients treated with REGN-COV2 versus placebo and more infusion reactions occurred with the high-dose REGN-COV2 compared with placebo (1.5% high dose, 0% low dose, 0.4% placebo).
Interestingly, the actual definition of the root word politic is: adjective – (of an action) seeming sensible and judicious under the circumstances. Although that definition seems incongruous with our national politics, it represents a prudent way to conduct our lives during COVID. Effective and safe vaccines with effective and safe treatments will end the nightmare of COVID but the relief they offer remains months away. Until they are a reality we must be politic in our actions and remain vigilant in mask-wearing and social distancing.
Updated October 21, 2020
In this week’s COVID update I want to focus on two issues that many of you have asked about, “reinfection” and “superspreading” made all the more real for me as they have impacted friends who are like family.
Many of you know that my wife, Iris, and I have been dividing our time between our homes in Atlanta and the North Carolina mountains. Our best friends in NC (G&M) are also from Atlanta but our relationship, to our son’s confusion, is only in NC making our time together there that much more special. Conflicting schedules had kept us apart for a couple of months and we were excited to be doing a physically distanced dinner on their outdoor patio two Saturdays past. We were driving up to NC that same Saturday morning when G&M called my cell to explain an inexplicable situation, their son (JB), who I’ve written about before, had just tested positive for COVID… a second time! JB first tested positive for COVID this summer when he was a camp counselor in a super-spreading event that made national news (more on that in part two of this update). Although JB was never symptomatic, he quarantined for two weeks, tested negative twice then donated convalescent plasma. When Georgia Tech recently reopened the campus he joined his fraternity friends who too had had COVID during the summer, albeit symptomatic. The fraternity participated in a campus-wide testing program which is how JB had just learned he tested positive again. Unfortunately, between the time of the test and the results report, he visited his parents resulting in the Saturday am call ending the possibility of the highly anticipated “safe” couples dinner. Literally one day later the first case of COVID-19 reinfection in the U.S. was reported in The Lancet Infectious Diseases: A 25-year-old man tested positive on April 18 and again on June 5; in between, he had two negative tests; during his second infection, he experienced worse symptoms and required oxygen. The two viruses causing the infections were genetically distinct, but both SARS CoV2. The key takeaways here are that despite general rules of post-infection immunity, reinfection is possible. But to be precise this isn’t a true case of re-infection, this is more akin to getting the flu despite having been vaccinated because the vaccine didn’t protect you from the mutated strain to which you were exposed. The prevalence of this virus, despite a relatively low mutation rate, has resulted in multiple strains emerging. JB’s asymptomatic infection vs his fraternity brothers’ symptomatic infection may have been the result of two different strains that did not convey mutual immunity. Such developments must give us pause and help us understand that neither natural herd immunity nor that achieved by vaccination, solves COVID and it is very likely that SARS CoV2-based equivalents to Tamiflu (treatment) and annual flu vaccination (prevention) may very well be our future COVID reality.
JB’s first COVID infection, when 85 of 300 camp attendees tested positive within the first week of camp, was among the earliest known examples of the phenomenon of super-spreading in which an event and/or individual is responsible for a large number of viral transmissions. Understanding patterns of viral transmission is a key tenet of disease management. Some of you have seen/heard mention of R-0 (pronounced R-naught), the epidemiologic notation for contagiousness or individual, “person to person” transmission. If on average each infected person infects one other person R=1. If a single infected person arrived at JB’s camp and infected 85 others is that an R=85 or is that oversimplified? Epidemiologists believe another measure, “K” (the pattern of dispersion) is needed to explain such a situation e.g., transmission at a population level. The concept behind K is based on an extensive contact tracing database which suggests that the vast majority of COVID transmissions can be traced back to <20% of the infected population (index patients). Such a situation was reported in this week’s MMWR in which researchers describe a COVID-19 superspreader event at a recreational men’s hockey game in Florida in June. The index patient, who was asymptomatic during the game, developed symptoms the day afterward. In the 5 days following the game, 14 of the 22 players plus a worker at the rink developed symptoms: and of the 13 who were tested, all tested positive. The concept of the index patient is supported by the fact that prior super-spreading studies have included viral genome analysis confirming in those studies that all involved were infected by the same strain of the virus. The concept of K highlights that super-spreading is a complex phenomenon in which multiple variables are in play: an asymptomatic carrier with high viral load, an environment conducive to spread (indoor, large gatherings, close contact, no masks, lots of respiratory aerosols), and possibly a more virulent strain of the virus. Since a person has to harbor the virus for a number of days before they too can transmit, such clustering of cases in a tight time period makes it less likely that it was simply a random event; it was not a coincidence that 85 campers all tested positive within a week of camp arrival each exposed by a unique person (R=1). Using measures like R and K help epidemiologists develop appropriate strategies to address both the common 1:1 viral transmission and the characteristics of the rare but more threatening super-spreading events.
So what to make of G&M’s tumultuous past 4 months or JB’s apparent bad luck, twice infected, or good luck, essentially twice asymptomatic. I see such stories as necessary reminders that as tired and angry and frustrated I may be with my current COVID lifestyle the rational response is to count to ten, take a breath, be thankful that no one I love has been hospitalized let alone died from this disease and put on my GD mask. I also remind myself that having come this far, with light at tunnel’s end in sight, it is not the time to risk it all. Masks and physical distancing work incredibly well while contact tracing can stop transmission in its tracks as we’ve seen in major league sports these past few months. I remain hopeful that such knowledge will inform a national consensus, but that’s for another update.
Best, Bruce
Updated September 21, 2020
“The vaccine will be ready by election day!”
“Effective nationwide vaccination is 12-18mos away!”
“The mask provides more protection than the vaccine!”
“Life does not return to normal until 2/3 of the US is vaccinated!”
These pronouncements, made in just the past 24hrs, make our heads spin and destroy our faith and trust in government, public health, medicine and the medical-industrial complex. What’s even crazier is that they are all correct. How can claims that on the surface appear to be direct contradictions all be accurate, that’s the topic for today’s update.
To understand the conundrum we have to understand the science. Vaccines are the product of medicine’s effort to mimic nature. In nature it is observed that following exposure to a virus, and the resulting infection, animals become immune to reinfection of the very same virus. This immunity is governed by the animal’s immune system producing antibodies to proteins unique to the virus. In most immune responses antibodies are made to multiple unique proteins; the lymphocytes recognize the virus, manufacture the antibodies and provide protection via a lifelong memory. Some viruses are genetically unstable and mutate constantly, making each exposure essentially a new disease with limited or no immunity e.g., Influenza. But, for many genetically stable viruses, those that do not routinely mutate, such immunity is lifelong – like measles. For mild non-threatening viral pathogens getting the infection is a simple way to achieve life-long immunity e.g., chicken pox, but for viral pathogens that have more serious consequences like polio and small pox, mimicking the body’s immune response through vaccination can provide the immunity without the preceding infection. The SARS CoV2 virus responsible for COVID-19 is another such virus.
With the above understanding the possible treatment strategies become clear:
- Get everyone infected like inviting kids to “Pox Parties” until the vast majority of the population is immune (herd immunity)-the problem here is that for as much as 40% of the US population COVID-19 infection is very serious and sometimes lethal-200,000 Americans have already died.
- Rather than develop the vaccine, harvest the antibodies from previously infected people or replicate the antibodies in the laboratory- although this is being done and may be a short term treatment strategy, antibodies denature in the blood in weeks to months; as a strategy this would require monthly, lifelong treatment.
- Create vaccines by using dead virus or viral proteins or viral RNA that when injected cannot infect and cause the COVID-19 disease but trigger the immune system to respond and produce antibodies to the SARS CoV2 virus as if the body were infected.
Injecting inactivated virus that cannot infect, viral proteins or viral RNA is not a simple endeavor and comes with risk. Even if the science has rapidly advanced such that we can unravel the genetics of the virus, identify the unique proteins and create a stable vaccine in months rather than years or decades, there still has to be testing to prove the vaccine is safe and effective. The proof of safe and effective begins in the chemistry lab advances to animal testing then to humans in three-steps or phased human subject clinical trials in which the vaccine is first proven safe (phase 1), then effective in generating an immune response (phase 2), and then effective in preventing infection without late unintended consequences (phase 3). Of the dozens of vaccine candidates about 10 have moved from the lab bench to animal testing through phase 1 and phase 2. One safety signal has arisen thus far with one vaccine (from AZ) for which research is on hold in US but has resumed in EU. Phases 1 and 2 need relatively few patients (as few as 20 to a few hundred) but phase 3 requires tens of thousands of unexposed volunteers to participate in a double blind experiment in which half are inoculated with the vaccine and half with a sham. Over a period of months to years researchers measure respective rates of infections and adverse events in the two groups. Based on statistical modeling, at preplanned intervals, the two groups are unblinded and infection rates compared (most of these trials were designed for 2yr surveillance). If there is statistical certainty that the vaccinated group was both protected from infection and didn’t suffer any untoward consequences, the manufacturer submits the data to the FDA for approval with hopes of subsequent distribution and mass inoculation. Even then the research is not done as those who are vaccinated continue to be observed and tested to determine the durability of their immunity e.g., will they need booster shots. Meanwhile the bench scientists continue tracking the SARS CoV2 mutation rates to determine if the vaccine stimulated antibodies will continue to prevent infection in the months and years to come.
Returning to the conundrum of contradictions we can see that an early (pre-election) interim analysis of a phase 3 trial by unblinding the two groups might show a meaningful difference that could result in a vaccine approval but it may be rightfully perceived as rushed to market and challenge the confidence of those in need. Purists will say that the trial needs to complete its course as designed but even then vaccinating a nation of 320 mil may take months or longer. Will everyone vaccinated develop an immune response? Will antibody testing be needed to prove such a response? Will masking and distancing be needed until a response is confirmed? How durable will the response be? If 50% of Americans refuse vaccination, as current polling suggests, will that prevent the herd immunity that wipes out this virus for good like polio and small pox or will SARS CoV2 remain a scourge for decades to come? Difficult questions that will not be answered before the election.
The conundrum of contradictions is a result of partial truths expressed in twitter and chyron sound bites that both oversimplify and obfuscate an incredibly complex situation. The contradictions are as much a creation of the way we obtain information and communicate as they are the biases and motives of those communicating. Know that in these difficult times the truth is there if you know how to dig for it. Know that masking and physical distancing is incredibly effective at protecting you. Know that there is a light at the end of the tunnel but it’s still unclear how far we have to go.
Best, Bruce
Updated September 11, 2020
It has been heartening to hear from many of you regarding the slowing cadence of my COVID-19 updates. Let it be known that I am neither a slacker nor a procrastinator. My lack of productivity has been simply the result of my belief that nine months into the pandemic I’ve said all there is to say. Then I remembered how you were there to listen when I needed a kindly ear to hear my concern that I had possibly contracted the virus and, worse, transmitted it to others. At that moment, I was not the physician, scientist, or teacher just a human being in need of human compassion. Empathy has never been my strength but even I understand that right now there is a need beyond the enlightenment of science and data.
We have fallen into survivable routines reminding ourselves how fortunate we are yet unsettled without an end in sight. We are starved for clarity; of thought, of vision, of reason while a constantly shifting landscape erodes our trust in science, institutions, and leaders. What we ask and what we need is a clear path forward.
Trying to see the forest for the tress and the path within has caused me to take a step back to focus on what we know, which after 9 months is considerable.
- SARs CoV2 is a novel coronavirus that has given rise to a disease syndrome COVID-19 (similar but more controllable novel coronavirus outbreaks e.g., SARS, MERS, have been arising every 5-10 years).
- COVID-19 infection is different from past coronavirus related infections as it may be asymptomatic or benign like a common cold but in some, especially the elderly, morbidly obese, and those with co-morbidities, it is a potentially lethal disease in which the immune and coagulation systems runs amok injuring heart, lungs, brain and other organs. (antiviral therapy-remdesivir, immune suppressants-steroids, and anticoagulants have dramatically reduced disease severity/mortality in hospitalized patients)
- SARS CoV2 is transmitted from person to person through viral particles we exhale. Although it is possible to acquire the virus from contaminated surfaces nearly all contact tracing studies show such transmission to be rare. (masks are critical to prevent person-to-person transmission and hand washing/sanitizing surfaces are easy albeit of limited value)
- The breath we exhale has both large vapor droplets which fall to the ground quickly (within 6 feet) but also tiny droplets (aerosol) which can float like a cloud in stagnant indoor air. (entering poorly ventilated crowded indoor spaces is like walking into a fog of virus)
- Viral transmission is directly related to the amount of virus exposure which in turn is based on the concentration of virus inhaled over time. (six feet distancing limits large droplet risk, masks limit aerosol risk but prolonged exposure e.g., in a classroom or in a bar, challenges the limits of these protections).
- SARS CoV2 is not a flu virus. It is not seasonal and, like all viruses, it mutates over time – but not with the speed of flu. (giving hope that prior infection or a vaccine will provide durable immunity of at least a year).
- Asymptomatic infection that may eclipse symptomatic COVID-19 by a margin greater than 10:1 raises the prospect of herd immunity (recent unsettling news coverage of waning antibodies after a few months, reinfections and 40% of the population being high risk with limited re-engagement significantly reduces the probability of herd immunity success).
- Vaccines appear to induce immune responses but are those responses durable, do they protect against infection, are the vaccines safe in both the short and long term and how will they be distributed to 320 million people are but a few of the questions that make the path forward anything but clear. (I’ll go in-depth on vaccines in next week’s update)
Although we have learned a great deal about COVID-19 in a mere nine months the extent to which this crisis has upended our lives and the realization of our vulnerability to natural events we cannot control has impacted our individual and collective psyche in ways that will not be clear for years. If these updates provide any comfort then I commit to greater consistency but I also ask your help. I want to know what topics you think need discussing and what clarity I might provide amidst the confusion. Please send your questions to Sam Garza to collate.
Best, Bruce
Updated August 10, 2020
Our dear friends have a son entering his sophomore year at Georgia Tech. He’s a good kid, responsible, solid values, industrious, compassionate. This summer was his last year of eligibility to be a counselor at one of the regional YMCA’s overnight camps. He was really looking forward to it and was ecstatic when Georgia was first to exit lockdown and the Y announced: “season on!” Day 4 of the first session he and four counselor friends tested positive for COVID, within two days 85 campers and staff, a third of the camp population, had tested positive as well. The camp closed six days into session and our friend’s son and his four buds quarantined together in one of the parent’s homes while the parents retreated to their cabin on the lake. Other parents made daily drop-offs of food, beer, and special requests while the boys set up a slip and slide on the back lawn, smoked pork butts and had some fun. They were still in camp mode just at a different campsite. To the best of my knowledge none of the boys or campers became ill, the vast majority remained completely asymptomatic. (Week’s later the regional camps re-opened across Georgia with the same outcome, hundreds infected within days.)
I tell the story now as the greatest issue we currently face as a nation in pandemic is school re-opening and I feel there are lessons from the camp scenario. It wasn’t as if the camp’s COVID surge and subsequent closure weren’t predicted, the debate was over its probability, timing and severity, which made for a good round of adult conversation over glasses of wine the week before camp started – no one guessed closure within seven days. The camp experience begs the question: why is the discussion binary, open or closed? Why couldn’t the camp have had parallel tracks, one for those with active virus and one for those without. Asymptomatic campers testing positive move into the active virus track until two consecutive negative tests then move back while campers who are symptomatic return home. This is the strategy being employed by major league sports (MLS, MLB, NBA) which has thus far, albeit only a few weeks, been successful. For the strategy to be successful the camp would need accurate, reliable, and rapid testing performed daily or every other day, which shouldn’t be so difficult if all the major league sports associations can do it. The camp would need to protect the adults in supervisory roles, but strong evidence published this week continues to prove the effectiveness of masks in preventing infection of the wearer, just as we see the coaches wearing in the dugout.
The described scenario suggests that if there is truly the will to re-open schools then there is also a way to do so that is rational and relatively safe. Yes, new data out this week has shown that children as young as five can harbor and transmit virus and that virus can live in micro-aerosol that floats in stagnant indoor air. An additional analysis published this week reveals the extent of lives saved when schools closed as a condition of initial lockdown. But we know a great deal more about this virus today than we did in March. The obstacles are not insurmountable as classes from August through October can be held outside throughout most of the US, while numerous other countries have proven that school-age children will wear masks and schools can test, track, trace and isolate those infected. If the US had a real strategy then schools would have the testing capabilities needed, the PPE and sanitizers for adult staff distributed and canopy tents for outdoor classes would have been sourced and made available at a reduced cost. Pilot programs could have been run during the summer to prove the strategy successful, thereby giving parents, teachers, and staff the confidence needed to support the process. A successful school re-opening strategy was possible, but it is likely too late to be deployed, and so we can discuss over glasses of wine the probability and timing of closure after a re-opening strategy that at best could be called wishful thinking. If only our nation valued its children the way it values professional athletes.
Best, Bruce
Updated July 21, 2020
I’m reading The Splendid and the Vile, Erik Larson’s latest work of non-fiction focused on Winston Churchill’s first days as prime minister. Churchill enters office as Adolf Hitler invades Holland and Belgium, Poland and Czechoslovakia having already fallen, and the Dunkirk evacuation just two weeks away. For the next twelve months, Hitler would wage a relentless bombing campaign on UK cities, killing 45,000 Britons, while U-boats paralyzed commerce and the supply chain and a land invasion seemed imminent. A different time, a different war, a different villain wreaking indiscriminate pain, suffering, and death on millions.
Depending on the definition of patient zero, we are now 6, 7, 8, or 9 months into the COVID-19 pandemic and the war waged against the novel coronavirus SARS CoV2. I’m finding it increasingly difficult to compose these updates as I feel I’ve already presented what needs to be said. In a post one month ago I predicted the current surge, its geography, age group, and lower mortality. This was not the result of extensive research, clairvoyance, insider knowledge, or a lucky guess. All that was required to make those predictions was a reasonable facility with basic math and a general understanding of the science of infectious disease.
Our colleague, Michael Smith, has spent his evenings and weekends developing models to predict the course of the pandemic with remarkable accuracy. If current trends continue his model predicts we may achieve the rudiments of herd immunity by the end of August. My last 5 years conducting real-world evidence research has taught me both the value and the limitations of healthcare modeling. Models are limited to the assumptions upon which they are built and can’t account for information that is in error or the vicissitudes of human nature and their influence on those responsible for public policy. At 15,000 new cases per day in just one state, Florida, restrictions get reimposed; when deaths double, or triple, lockdowns get re-instituted; irrespective of public policy, fear will reverse re-engagement for many. If parents won’t send their children to school and those over 60 self-quarantine the economy stalls, the possibility of herd immunity fades and the pain, suffering, and death of so many will be in vain.
I hope and pray that, if the assumptions are correct and public policy doesn’t change, Michael’s model is accurate and we exhale a sigh of relief come September. But as the wise men say “hope is not a strategy” and “triumphs of hope over reason” make good fiction. All of which brings me back to Larson’s book on Churchill in 1941 London during the blitz. His indomitable spirit is a lesson to all of us as we persevere in these most unique and difficult times.
Because the news of the past few days warrants the salve of humor I offer the word of the week — Coronacoaster (noun): the ups and downs of a pandemic. One day you’re loving your bubble, doing workouts, baking banana bread and going for long walks and the next you’re crying, drinking gin for breakfast and missing people you don’t even like.
Best, Bruce
Updated April 10, 2020
My father had a small retail clothing business in Philadelphia. Twice a year he would drive north to the garment district in NYC for the next season’s apparel buy. These trips morphed into family weekend getaways. Driving north we’d cross the Delaware line into New Jersey near Trenton over a bridge that was emblazoned in 20 ft high letters spelling out “WHAT TRENTON MAKES THE WORLD TAKES.” Yes, it was a global economy in 1966. If America is to be open for business, the world needs to be open for business.
The headlines may make this proposition seem unattainable yet I am optimistic. Immersed as we are in this first phase of the pandemic in which we pray daily for new case activity to peak as daily death counts rise we need to be ever cognizant that the present is the past and our focus must be on the future. The future is the next phase (2) of the pandemic in which recoveries exceed new cases, immunity allows for social re-engagement, tracing allows isolation of newly infected who receive appropriately timed treatments that lessen disease severity.
In the next four weeks the US and the rest of the industrialized world should: see social distancing flatten the curve; have readouts on a half dozen clinical trials evaluating the effectiveness of treatments (chloroquine, hydrochloroquine, remdesiver, convalescent plasma); likely have three approved accurate serologic tests (antibody assays) that can determine immunity and have the data to more effectively characterize high-risk populations. With this data and these tools Phase 2 is conceivable. We can begin to explore scenarios in which those who are immune can fully re-engage without risk to themselves or others. We can define the high-risk individuals who must continue to isolate pending a vaccine or treatment that conveys the equivalent protection from the risk of severe illness. Immunity passports can be issued to those who have antibodies while those at low risk can re-engage as long as they undergo frequent testing for viral RNA and if positive isolate and trace contacts.
Trenton may no longer be a hub of manufacturing but the global economy it recognized a century ago is in full effect today. For America to be open for business the world must also be open. International agreement on how to re-open with the least risk of a second surge will require acceptance of measures that impinge on our personal freedoms. We were successful in doing this after 9/11 and I am optimistic we can be successful again.
Best, Bruce
Updated April 2, 2020
It may seem that the Pandemic has been with us since December, but most of us have only just completed the second week of sheltering at home. My last business trip concluded just three weeks ago on March 8. Social media abounds with commiseration for the shared experience of running out of Netflix shows to watch, but for some like me, that happened months before COVID-19. We want to believe that this will be over soon, but such thinking begs a triumph of hope over reason. Our shared reality is that the pandemic in the US has just begun and we need to be prepared for months of sheltering but not necessarily social isolation. This doesn’t mean we can’t dream of a resumption of some new form of normalcy, but for that to happen we need modeling that confirms the risk of doing so will not make our shared situation worse. Such talk of re-opening America for business has generated a great deal of recent conversation which is what I wanted to focus on in today’s update.
America being open for business is a catchy phrase but in the COVID-19 era it’s quite complicated. One way of thinking about the economic engine of the US is to think of the consumers and producers, and one way of measuring them is by age group. Amazingly the US population, divided into age deciles i.e., <10, 10-19, 20-29, … 70+, reveals the population to be near equal in each decile approx. 40mil.
- The first two deciles comprise 80 mil Americans, specifically those 19 and younger who have limited direct impact via the purchase or creation of goods or services.
- The last two deciles (age > 60), also 80mil, have limited contribution to the production of goods and services, but they do consume, especially in hard-hit market sectors like travel and leisure, retail, restaurant, and hospitality. Unfortunately, this group has such a high risk of devastating health outcomes if infected with COVID-19 that they will not be able to fully participate in an open America until there is a vaccine or its therapeutic equivalent.
- The remaining middle four deciles (160 mil), half the population, are the core of the economic engine and the group that might re-open America. Unfortunately, many of them have risk factors e.g., diabetes, obesity, chronic disease, smokers, etc., for whom participation may be too risky. Furthermore, many of this group are already working in market sectors that are not siloed by the pandemic because they are deemed essential or are using telework e.g., healthcare, technology, communication, e-tail, food production/grocery/drug store, logistics, government (military, police, sanitation), service e.g., electrical, plumbing, HVAC, landscape, construction.
- Of the remaining population aged 20-60, their personal risk from COVID-19 may not be much worse than influenza in a bad year, but their risk to those who are elderly or compromised may be significant.
All of this begs the question of who will re-open America and how can they mitigate risk effectively?
Mitigating risk requires more data than we currently have and that data requires testing not currently deployed or accessible. Those who are more than four weeks out from exposure to COVID-19, either asymptomatic or symptomatic, will likely have developed an immunity. Immunity can be proven with blood testing for appropriate IgM antibodies. A five-minute blood test by tabletop analyzer was just approved by the FDA, but projected capacity is only five million tests a year and we’ll need 10-20x that number.
- If immune, you have no risk of reinfection, but more importantly you can’t transmit. These folks can engage in the economy with abandon, they can also be on the front line directly engaging with those who are symptomatic with infection or at high risk. They can even donate plasma that can be used to treat the sickest.
- Those 20-60 y/o low risk who are not immune, but without active infection as determined by testing for viral RNA by nasal swab, could engage as their risk of serious complications from infection is low. However, should they become infected, they could transmit disease to others who are more vulnerable. Because of this, these folks need to be tested for active disease often e.g., weekly and, when positive, isolated.
Currently, too little time has elapsed to allow for a large segment of the population to be immune but this will change quickly in the coming two to three months. Hopefully, by then we will also have effectively deployed testing for both viral RNA by nasal swab and immune status by blood testing to make re-opening America, for at least a portion of the population, a safe possibility. When America re-opens for business we should be clear that this is not a return to the old way of doing business. America during the pandemic may be very different than the America we’ve known, but the America post-COVID is likely to be very different as well.
More thoughts on re-opening America in the two accompanying essays.
- We Can Safely restart the Economy in June. Here’s How: https://www.nytimes.com/2020/03/28/opinion/coronavirus-economy.html?referringSource=articleShare
- It’s Too Late to Avoid Disaster, but There Are Still Things We Can Do: https://www.nytimes.com/2020/03/27/opinion/coronavirus-trump-testing-shortages.html
Best, Bruce
Updated March 13, 2020
In the week since I last posted about the coronavirus disease, labeled COVID-19, it has landed on our shores. Thousands are likely infected and tens have died. It’s real, it’s here and it will be with us for a while. Information and misinformation about the spread and containment, speculations and accusations about the severity and response, continue to dominate headlines. I will once again try to provide a factual and rational summary of the current knowledge based on my analysis of CDC, WHO, FDA and other reports as well as insights from Infectious disease specialist colleagues.
- Name – COVID-19 is the disease caused by the coronavirus strain now dubbed SARS-CoV-2 despite the fact that COVID-19 virus is only 30% homologous with the SARS coronavirus. COVID-19 is not SARS but they are both coronaviruses
- Risk – Population tracking studies are beginning to clarify risk groups, and risk directly correlates with age and prior lung disease which includes smoking. Children < 15 appear to get mild if any symptoms. Young adults similarly get mild flu-like symptoms. Middle-aged adults, in particular male smokers, have more risk of severe consequences. Those over age 70, particularly those with chronic diseases, especially lung disease, may have as much as a 10% mortality risk. Immunosuppression e.g., cancer treatment, may not significantly increase risk.
- Disease Pattern – average time from exposure to symptoms is 5 days, symptom development after 12 days is rare, this is the basis for the 2wk self-quarantine if you’ve been potentially exposed. Flu-like syndrome (fever, aches, fatigue, dry cough) are the initial symptoms lasting 5-7 days. Shortness of breath, if it develops (20%), does so after day 7 – with a 50% chance of requiring hospital care.
- Testing – Among the most limiting factors impacting our current knowledge is the lack of available, rapid and accurate testing. Why we don’t have testing will be hotly discussed in the coming weeks and months but what’s important to know is that we won’t understand transmission and lethality without adequate population testing. Experts all hope that testing will be routinely available by 4/1
- Treatment – there have been few good-news stories since this crisis broke but one is Remdesivir, a broad-spectrum antiviral drug that is active against RNA viruses like Coronavirus. It was developed for SARS and Ebola. Like drugs, for AIDS it lessens viral activity and viral load. It may not be a cure but if the preliminary research is validated, taking Remdesivir at the onset of symptoms may prevent progression to the severe and potentially lethal respiratory disease that emerges in week two of infection.
- Containment – 30-second hand scrub is the most effective hand sterilizing technique. >60% alcohol sanitizers may work, some viruses like coronavirus are membrane-bound (i.e., norovirus is not), >60% alcohol disrupts the membrane and destroys the virus, but studies have not been done so only substitute is you can’t scrub. Clorox wipes, among others, will decontaminate surfaces but the surface must stay wet after wiping for 60sec ( e.g., plane seat/armrest/ tray), do not use on skin.
- Transmission – is person to person and infected individuals can transmit before they have symptoms. Without symptoms, they won’t be coughing in your face so masks don’t help but they may be shaking your hand with a hand that just touched their mouth, eye or nose. Don’t shake hands, try to keep a reasonable distance (6 ft recommended), wash your hands vigorously and often AND DON’T TOUCH YOUR HANDS TO YOUR FACE. Kids may not be at risk but they can be a vector for disease transmission, that’s one reason behind school closure.
- Understanding infectious disease spread may be scary but we need an eyes-wide-open approach, especially as our business will be critical to our nation’s success in dealing with this crisis. If no measures were taken to disrupt the spread then every 5 days each infected but asymptomatic person might infect two other people then those folks each infect two others and so on. If you apply exponential math based on 2000 infected folks in the US today, then there’d 1 million U.S. cases by the end of April; 2 million by May 7; 4 million by May 13; and so on. If only 10% needed hospital care that caseload would overwhelm our healthcare system. That’s why China, South Korea, and Italy essentially moved to national self-quarantine and it worked. That’s also why leadership today announced a no-travel policy.
Hopefully, testing, containment, and effective anti-viral therapies like Remdesivir will stem the tide of caseloads until we have a vaccine. AND DON’T TOUCH YOUR FACE!
Please see the following article from Vox – How canceled events and self-quarantines save lives, in one chart.
Best, Bruce
Published March 6, 2020
To My WCU listeners,
Like you, the continuously evolving news about Coronavirus (COVID-19) is incredibly unsettling for me, my family and loved ones. I find what I don’t know to be even more unnerving than what I hear and read. I’ve summarized my research to share with those I hold dear to help them confront this moment rationally and with the belief that being informed is being armed. Please share this with your friends and loved ones.
What’s the difference between a viral infection and the flu?
There are hundreds of thousands of viruses that infect nearly all living creatures. Many that infect humans are well-known likes measles, mumps, flu, and the common cold. A virus, like influenza, is not one thing, it’s more like a family of related viruses with each unique member of the family being just one strain of the virus, e.g., each year a new strain of flu requires a new vaccine
Unlike bacteria, which can be treated with antibiotics, viral infections are difficult to treat but they can be prevented with vaccines. If you get exposed to a virus your body’s immune system will keep a memory against it which prevents re-infection.
Vaccines mimic the body’s immune process by creating a memory but without the symptomatic infection. When a new virus emerges, usually because it jumps from an animal host to humans, no prior human exposure means no immunity in humans creating a risk for the virus to spread like wild-fire, which is called a pandemic.
What is COVID-19?
Coronavirus has been known for decades as a cause of the common cold, but in 2003 and again in 2012, two much more serious strains arose by jumping from animals to humans, they were called SARS and MERS. Fortunately, they did not spread wildly and were both quickly contained, but their lethality contributed to the initial panic reaction to the emergence of COVID-19.
The Coronavirus disease that emerged in Wuhan China in late December 2019, now called COVID-19, is such a virus. It is a species of coronavirus that jumped from bats to humans. We still don’t know enough about COVID-19: we don’t know how lethal it really is. The annual flu epidemic has a 0.2% mortality (2 deaths per 1000 infected). We know that because testing for flu is easy and available. Thus far COVID-19 testing is limited, and only those who are symptomatic and needing healthcare are being tested.
It may be that it is 10 times more lethal than typical flu OR it may be that 9 of every 10 people who get infected get no symptoms or just a cold, aren’t tested, and the mortality rates are overestimated. Lethality is also related to how easily the virus is transmitted. Unfortunately, we now think COVID-19 can be transmitted by infected people before they have symptoms like fever and cough.
Who’s at risk of COVID-19?
We are not all equally at risk. Most deaths have been in the elderly, frail and chronically ill. No reported deaths in children < 15. Since there is no specific treatment, and it may take 6-12 months to develop a vaccine, there are a limited number of things we can do as individuals, as communities, and as nations to limit the spread:
- quarantine communities where the infection is rampant (that might include travel restrictions, school closures or event cancellations)
- hand washing (sanitizing) and keeping hands away from your face so the virus doesn’t get into nose, mouth or eyes
- only wearing a high quality (N95) mask if in contact with those infected/coughing.
It may turn out that COVID-19 is no worse than a bad influenza season. But because this virus is new to humans, and we have so much more to learn, the fluidity of the situation is creating significant unease. As research answers more of the critical questions, I’ll provide updates as needed. Taking these preventative measures from the CDC is recommended.
Best, Bruce